CONTACT: 877.333.4499

|
CONTACT: 877.333.4499 |
|
Making Critical Hospital DecisionsUsing ProModel Simulation Technology
Special Note: Carilion Clinic has strictly used MedModel Technology for the purposes of this analysis.
|
Carilion Healthcare's Process Improvement Team chose ProModel's Simulation Technology to reduce hospital overcrowding and resolve patient flow issues.
Hospital overcrowding can be a serious problem! Lack of inpatient beds is one of the most significant concerns for Hospitals, particularly Emergency Departments. Lack of in-patient beds threatens patient quality of care and safety. It also threatens a health system's bottom line. The Affordable Care Act (ACA) has increased the insured base and hospital overcrowding is likely to become an issue for Carilion, as well as the rest of the nation's hospitals. Carilion has built models of several of its hospital systems. This story focuses on just one.
A complete model was built and a baseline scenario simulation was run. Experimental scenarios were defined over an extended period of time as part of an on-going census management project. Throughout the project, different hospital staff, the Census Management Steering Committee, came up with different ideas on how hospital efficiency and patient flow could be improved. These ideas resulted in many different experiments which were conducted using this hospital patient flow model. Just a few of these experiments and the resulting decisions are further explained here. Carilion tested multiple others and continues to do so.
If you would like more information about how ProModel can help you make critical decisions about your Healthcare Organization contact us @ 877.333.4499 or HealthcareSolutions@ProModel.com.
1. Should We Set Aside Unit 7E?
2. Should Hospitalists Be Given Priority to PCU Unit 8W?
3. Should We Expand 7W to 24/7 with 16 or 20 Beds?
4. Should We Establish a Suicide Prevention Unit?
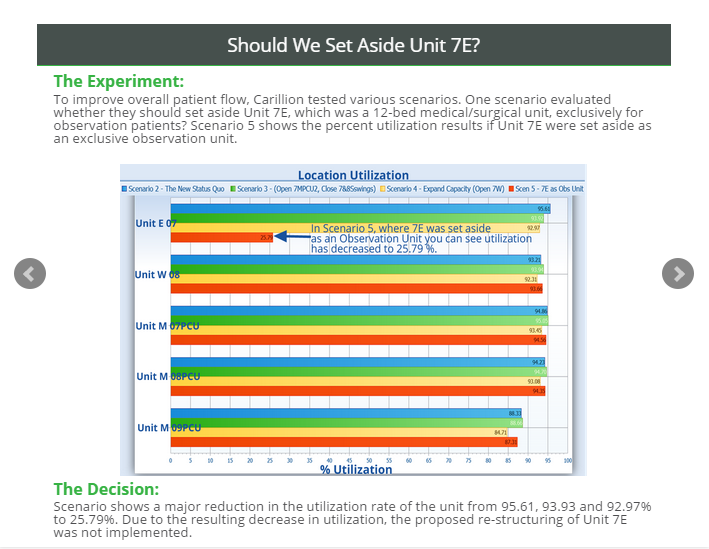
To improve overall patient flow, Carillion tested various scenarios. One scenario evaluated whether they should set aside Unit 7E, which was a 12-bed medical/surgical unit, exclusively for observation patients. Scenario 5 shows the percent utilization results if Unit 7E were set aside as an exclusive observation unit.
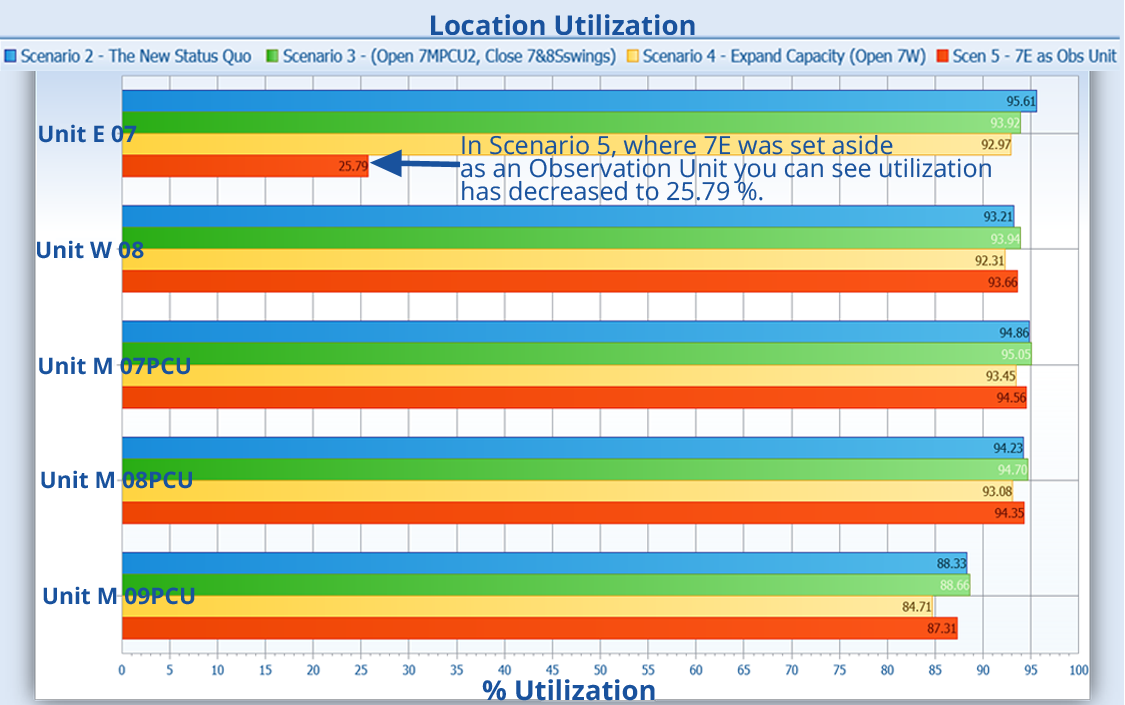
Scenario shows a major reduction in the utilization rate of the unit from 95.61, 93.93 and 92.97% to 25.79%. Due to the resulting decrease in utilization, the proposed re-structuring of Unit 7E was not implemented.
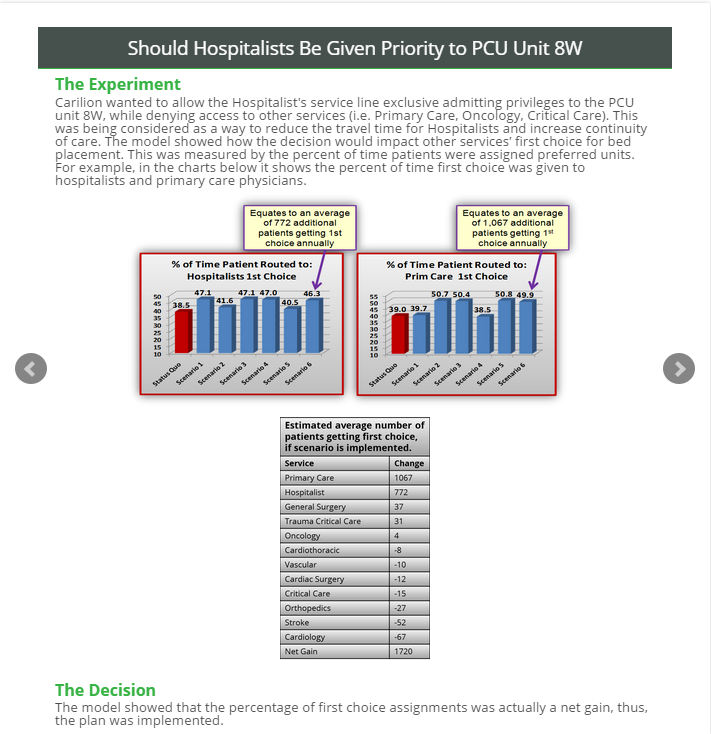
Carilion wanted to allow the Hospitalist's service line exclusive admitting privileges to the PCU unit 8W, while denying access to other services (i.e. Primary Care, Oncology, Critical Care). This was being considered as a way to reduce the travel time for Hospitalists and increase continuity of care. The model showed how the decision would impact other services’ first choice for bed placement. This was measured by the percent of time patients were assigned preferred units. For example, in the charts below it shows the percent of time first choice was given to hospitalists and primary care physicians.
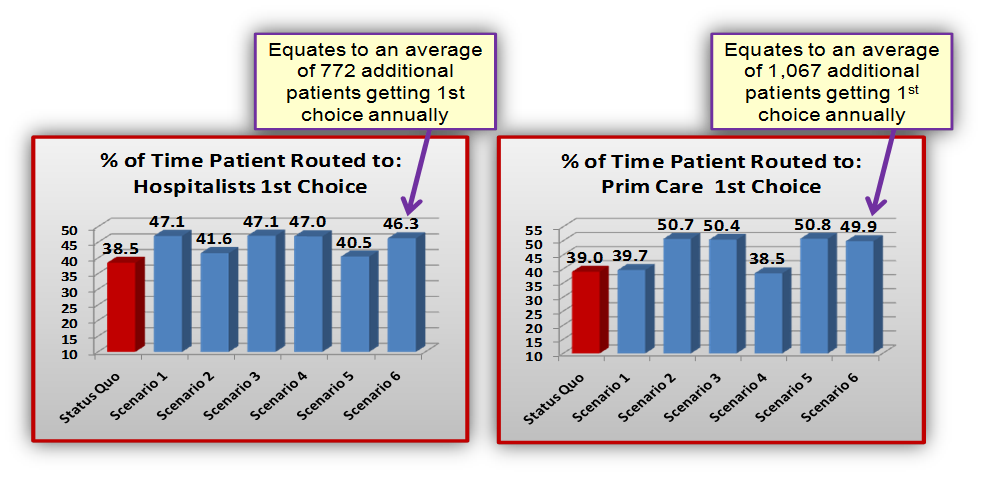
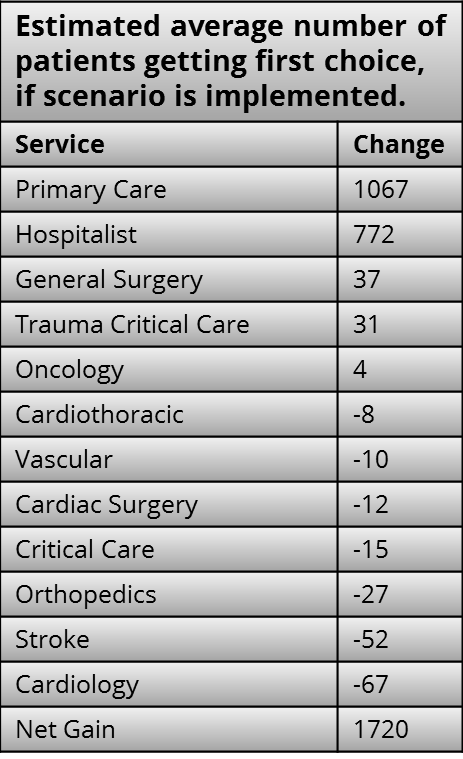
The model showed that the percentage of first choice assignments was actually a net gain, thus, the plan was implemented.
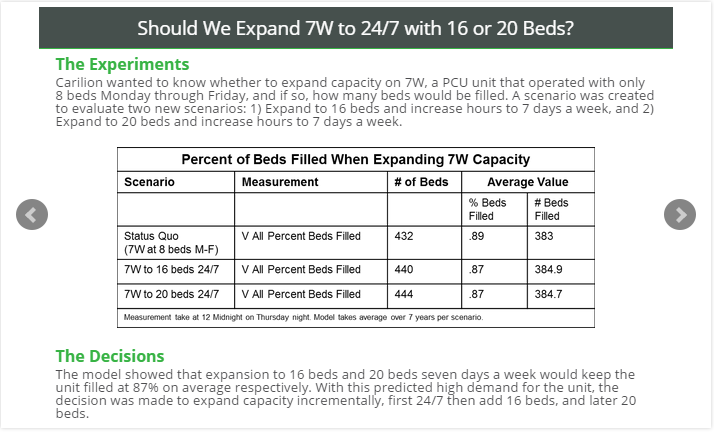
Carilion wanted to know whether to expand capacity on 7W, a PCU unit that operated with only 8 beds Monday through Friday, and if so, how many beds would be filled. A scenario was created to evaluate two new scenarios:
1) Expand to 16 beds and increase hours to 7 days a week, and
2) Expand to 20 beds and increase hours to 7 days a week.
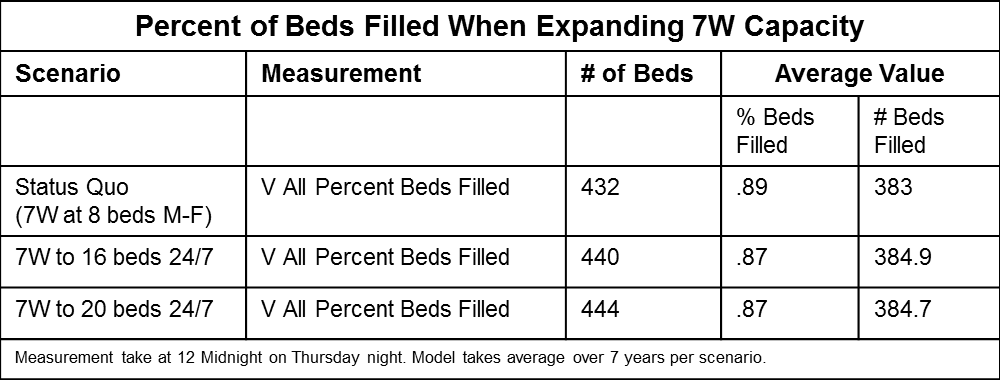
The model showed that expansion to 16 beds and 20 beds seven days a week would keep the unit filled at 87% on average respectively. With this predicted high demand for the unit, the decision was made to expand capacity incrementally, first 24/7 then add 16 beds, and later 20 beds.
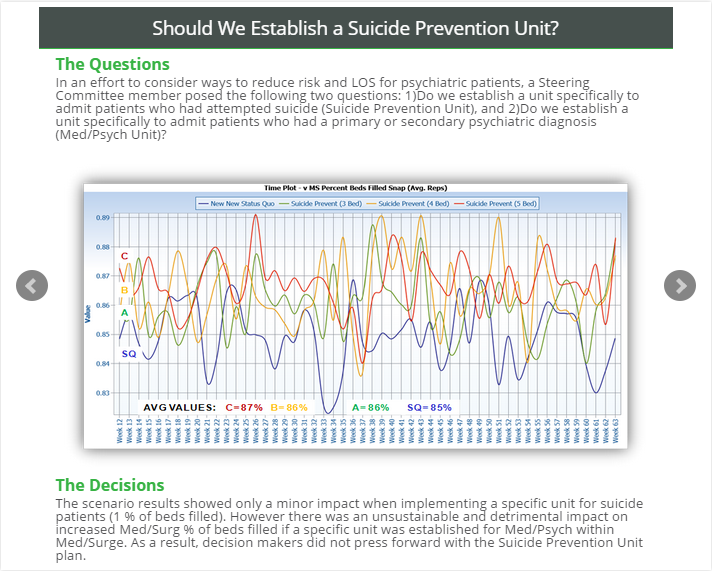
In an effort to consider ways to reduce risk and LOS for psychiatric patients, a Steering Committee member posed the following two questions: 1)Do we establish a unit specifically to admit patients who had attempted suicide (Suicide Prevention Unit), and 2)Do we establish a unit specifically to admit patients who had a primary or secondary psychiatric diagnosis (Med/Psych Unit)?
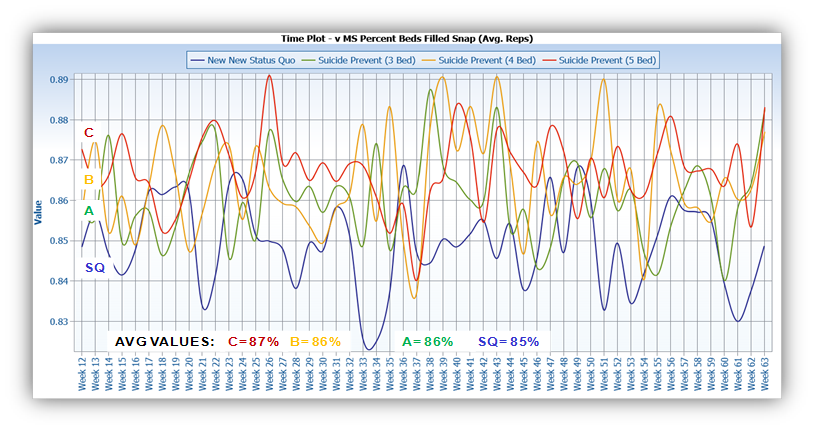
The scenario results showed only a minor impact when implementing a specific unit for suicide patients (1 % of beds filled). However there was an unsustainable and detrimental impact on increased Med/Surg % of beds filled if a specific unit was established for Med/Psych within Med/Surge. As a result, decision makers did not press forward with the Suicide Prevention Unit plan.
A Not–for–Profit Health Care OrganizationCarilion Clinic is a comprehensive network of hospitals, primary and specialty physician practices and services in the state of Virginia. The entire organization services 1 million customers in 23 counties. There is one Tertiary Care Facility and 6 Acute Care Community Hospitals with a total average daily census of 630.
James B. Montgomery, Senior Performance Improvement Consultant at Carilion Clinic and a Certified Six Sigma Black Belt, worked with ProModel consultants to create the Hospital Patient Flow Model for the Roanoke-based tertiary care medical center. This story represents the patient flow analysis and improvement in that facility. ProModel's unique discrete-event simulation technology (DES) predicts complex system outcomes and is the best tool for studying hospital systems with their incredible amount of variability and the interrelationships between staff, units and patients.
This Hospital Patient Flow Model allowed decisions-makers to easily play "what-if?" analysis with a host of proposed policy changes to nursing unit capacity and judge the impact on desired output variables in order to make the right decisions prior to full implementation of those decisions. If you would like more information about how ProModel can help you make critical decisions about your Healthcare Organization contact us @ 877.333.4499 or HealthcareSolutions@ProModel.com.
|
|
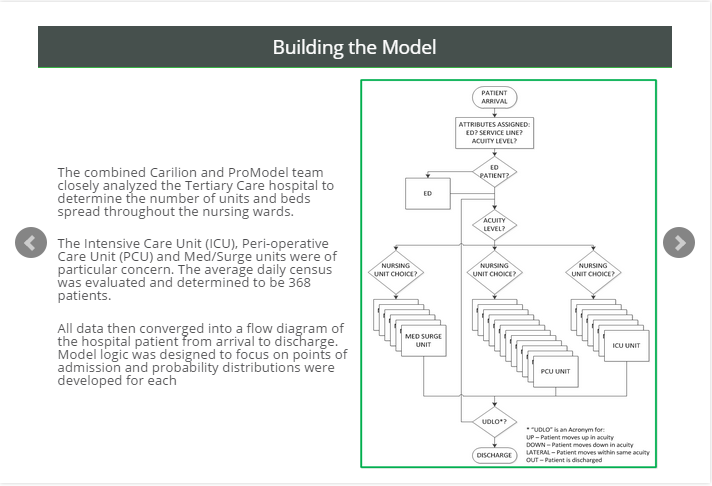
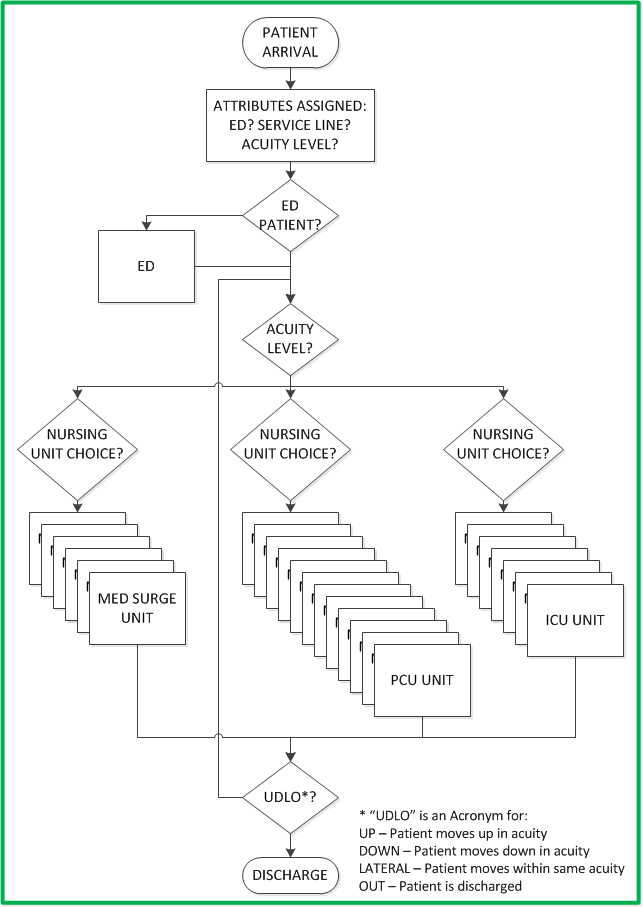
The combined Carilion and ProModel team closely analyzed the Tertiary Care hospital to determine the number of units and beds spread throughout the nursing wards.
The Intensive Care Unit (ICU), Peri-operative Care Unit (PCU) and Med/Surge units were of particular concern. The average daily census was evaluated and determined to be 368 patients.
All data then converged into a flow diagram of the hospital patient from arrival to discharge. Model logic was designed to focus on points of admission, and probability distributions were developed for each unit.
|
|
|
Next, the service line of the admitting physicians was considered, as well as patient acuity levels.
Multiple routing sequences were created based upon these two attributes.
Two years of admissions data were analyzed to design the correct model logic.
Data were also gathered from interviews with various hospital personnel. 109 possible Length-of-Stay (LOS) distributions resulted.
|

|
According to Harvard Business Review, Walter Frick; FEBRUARY 27, 2015, People Trust Human Judgment Over Algorithms, which is another reason it is critical to perform model validation.